4th April 2024
This is the second article in a series describing the impact of technology on the care and support sector.
Summary
TEC applications and services will move quickly away from alarms and rely increasingly on data obtained from a wide range of sources including sensors, apps and connected devices, electronic health records, and unstructured sources such as video images, and interactions with people, devices and equipment in their homes.
TEC delivery services will also generate data from records of use, responses to alerts and requests for help, and the outcomes of interventions. Data analysis will inform more sophisticated and holistic models of health and wellbeing enabling timely changes to be introduced to support individuals in their day-to-day lives or respond to sudden changes in need. Monitoring platforms will need to develop their capabilities so that they can initiate and coordinate responses.
Introduction
In our previous article, we presented a landscape review of technology-enabled care (TEC) in the UK. It described five generations of TEC that began with basic reactive alarm services for risk management, and which have evolved into a data-led approach, enabling proactive and predictive models of support that can provide timely and context-aware interventions. We concluded by saying that next-generation technologies will disrupt how care services are configured, allowing them to take full advantage of the opportunities offered by a truly integrated digital care platform.
This shift, which is driven, in part, by the digitisation of the UK’s telecommunications networks, can be considered as a move away from a ‘just in case’ safety-net approach to one that offers ‘just-in-time’ support. Thus, a blended or hybrid model of care is envisioned – with technology-enabled ‘ambient assisted living’ seamlessly augmented with people-based services, as required. In this article, we consider in more detail the increasing role of data and its collection in these services.
Changing service models
First and second-generation alarm-based telecare applications support people to live independently at home. They use wireless alarm pendants and sensors to transmit an alarm signal to a hub in the home. The hub forwards this alarm on to a monitoring service and a call handler responds accordingly by providing reassurance and arranging a suitable response. Support is also available when outside of the home by using mobile devices such as GPS alarm pendants that can raise an alarm, enable two- way speech, and provide location information to a responder, as shown in Figure 1. The latter is especially important for supporting people with dementia who may become lost and require assistance to return home safely. Services are entirely reactive in nature
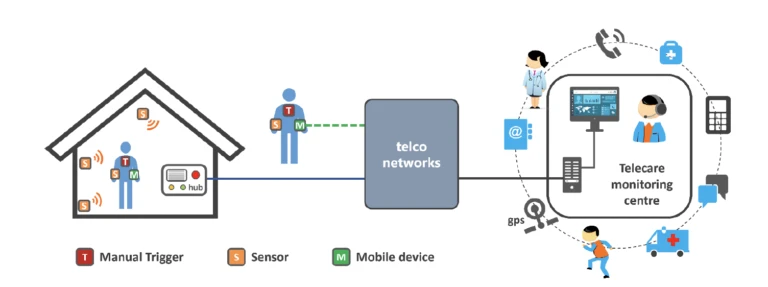
Figure 1: Basic overview of 1/2G telecare applications.
Third generation applications and above are based on their ability to monitor the activity (or inactivity) of a person to provide information about their daily routines, general safety, wellbeing, and interaction with others. Activity monitoring relies mostly on sensors installed in the home, as they are primarily aimed at supporting people who spend a lot of their time at home by themselves. Wearable devices are increasingly being used to complement home-based monitoring, adding additional activity and health data whilst also extending the monitoring when they are outside of the home.
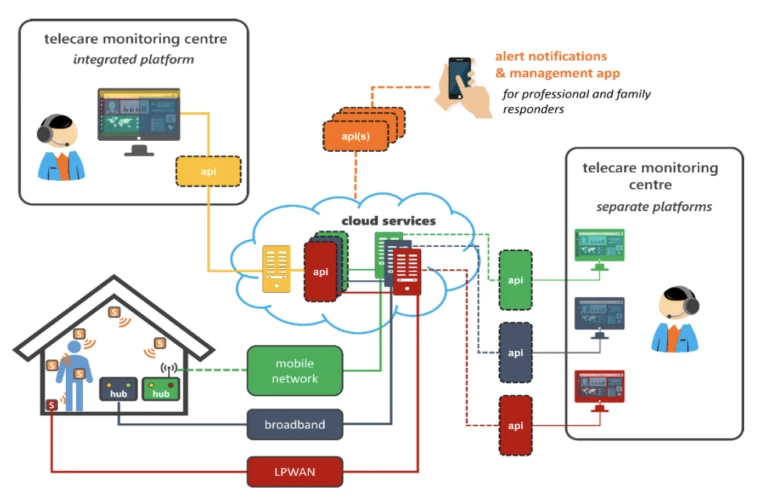
Figure 2: Multiple 3G+ applications each with their own technology stack and user interface.
The core elements that make up a typical 3G+ applications are shown in Figure 2. Sensors in the home transmit data wirelessly to a data hub which uses a broadband or ‘wireless’ data connection to upload it to a cloud-based server. From there it can be viewed using a data dashboard; rule-based alert notifications can be sent to a smartphone if there is an issue that requires an intervention or response – perhaps by a family member, mobile warden or domiciliary care service. These can be sent BEFORE an emergency occurs. In some cases, the systems allow an alarm to be forwarded to a monitoring centre so that a call handler can respond and organise an appropriate response.
Activity monitoring is typically used in two modes of operation:
- Daily activity assessment – a means of establishing an individual’s behaviour over a period ranging from a few days up to several weeks to build-up a better picture of their daily routines, capabilities and reliance on family and other visitors (or carers) so that a package of care can be designed that best meets their needs, or to justify an existing level of support; and
- Safety reassurance – monitoring an individual’s behaviour constantly to keep track of how well they are coping with their everyday tasks, including the safety and security of the home; the systems have the ability to notify a responder if there is a problem.
Daily activity assessment helps to establish the daily routines of individuals so that packages of care and support can be better matched to their specific requirements. This mode of operation is often used to help design reablement packages for individuals who have been discharged from hospital. It offers objective data on the movement levels and the activities undertaken by individuals in their own home to help establish the best package of care to support that individual to remain at home successfully. For this reason, it is also used in supported living to ensure that support arrangements are well-matched to the needs of each of the residents. It can be used to answer questions such as:
- Are night staff needed?
- When are service users managing independently?
- Are some service users effectively losing some of their independence to compensate for the greater needs of one or two housemates, and
- When are staff having the greatest effect?
Safety reassurance works by establishing a baseline picture of an individual’s daily activities. Any significant changes from this norm could indicate that a timely intervention may be beneficial to help prevent a decline in their capabilities or long-term health, thus supporting the person’s wellbeing and prolonging their independence. Some changes may also indicate a potential emergency, requiring an immediate response – thus there is some overlap with traditional telecare services. One key difference though is that the responder may be a family member or support worker receiving a notification directly on their smartphone rather than through a call handler in a 24/7 alarm monitoring centre, although the latter is available as an option for some products. This mode of operation can also support assessment applications – the key difference is the ability to generate alerts based on rules.
The inclusion of multiple sensors, smart devices, and data from other sources e.g. local weather conditions, electronic health records, and ‘big data’ makes them more capable of supporting preventive services. In practice, a service commissioner/provider may rely on technology from multiple vendors, each with their own technology stacks, as shown in the monitoring centre configuration on the right of Figure 2. This is far from ideal as it involves switching between multiple platforms and added value may not be realised when data residing on different platforms cannot be easily combined for analysis. From a commissioner/provider’s viewpoint, a single integrated platform capable of presenting a single source of truth for the entire data model offers much greater potential; this is shown in the monitoring centre on the left of Figure 2. The ability to achieve this level of integration depends on the willingness of the monitoring platform provider and each of the technology providers to work together, and to demonstrate that this can be achieved.
Data from Sensors
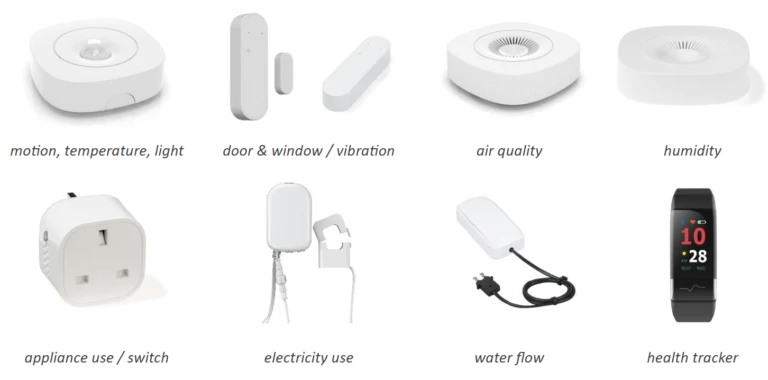
Sensors for data gathering in 3G+ applications are installed in the home and on the person being monitored in the form of wearables (or devices carried in a pocket/bag or attached to a keyring). Sensors measure one or more parameters such as temperature, humidity, light levels, gas concentration, sound and movement which are all relevant to a landlord and their responsibility for a healthy, energy-efficient home free of damp. Activity detection is important for both social care and rehabilitation following a health incident, but it is not simple to monitor because of the need to track behaviour and the performance of all types of domestic activity. This has led to the development of proximity and interaction sensors from which the type of activity can be deduced. The use or status of electrical devices can be monitored directly with plug-in devices or through an analysis of power use through a smart meter or a power clamp device on the electricity input to the property. Water flow detectors can be used to differentiate between the flushing of the toilet and the opening of taps, for example. Sound and vibration sensors can be embedded in walls or furniture or into the flooring to detect impact, monitor gait, occupancy, or other routine sounds such as music, or emergency cries of distress. Figure 3 shows a selection of IoT sensors that can be used in 3G+ applications, many of which offer support for multiple parameters e.g., motion sensors often also detect ambient light and room temperature. They are increasingly manufactured as low-cost generic devices from companies such as Develco, Fibaro and Sensative. Ikea are planning to launch their own versions of many devices.
In addition to these, there are also new devices that use imaging technologies with on-board processing to determine activities and to identify adverse incidents such as falls. This method, used by Nobi Lamps and by Sensio, may increase the acceptability of video monitoring in areas where people may have privacy concerns, Figure 4.
Monitoring using microwave radar imaging, as used by Vayyar, might also be less intrusive. Whilst some systems offer additional functionality (such as cough monitoring with the Nobi lamp), others are single-purpose and remain alarm-focused. These sensors can, in principle, be integrated into 3rd generation activity monitoring systems as additional inputs. In all cases, privacy and confidentiality concerns of end users and their families need to be considered from an ethical perspective. Issues relating to cyber-security should be designed into the technology stack.

Major telecare vendors invested in telehealth companies so that they might employ their monitoring platform software to remotely manage patients with long-term conditions, following the benefits shown in the Whole System Demonstrator project in 2011. Their popularity waned but the idea of remotely collecting vital signs data to manage the health of people with chronic obstructive pulmonary disease, and circulatory diseases, has become a priority. It drives both Virtual Wards and more general monitoring and support schemes to empower people to use peripheral sensor devices of the type shown in Figure 5 to report their results using messaging applications or an app. The devices have already become commodities that are available as consumer products. New devices continue to be developed. Ingestible and implantable medical devices lie outside the scope of this article, but will undoubtedly add to the data that will be routinely available for use in smart systems.

Figure 5: Devices for home physiological monitoring.
Finally, the increasing popularity of wearables that provide continuous health and activity monitoring will also provide important data. Products such as Google’s Fitbit and the Apple Watch provide simple activity and step tracking. The Apple Watch, for example, also provides high/low and irregular heart rate notifications, ECG monitoring, mobility, and cardio fitness, fall detection, and medication reminders. The Fitbit Sense 2 measures stress. Information from these devices, which may be owned by individuals, will increasingly become available for integration with technology-TEC applications.
Extended data sets
4G+ technology-enabled care applications can benefit from data obtained from wider sources, such as local weather conditions (temperature, humidity, pressure, rainfall/snow, wind speed, etc) as well as air quality readings (e.g., looking at pollution and pollen levels). Data from household wastewater monitoring can help to determine the spread of Covid-19 in an area. Information such as local travel conditions and public transport information might also be of use more generally. Looking to the future, it may be possible to incorporate large amounts of unstructured data from additional sources such as image-based sensors, voice user interfaces or other interactions with people and machines – and not constrained to the home – so-called ‘big data’. An attraction of using ‘big data’ is that it can be collected without having to install bespoke sensors into a property. Installation and maintenance of sensors will become increasingly important as more data sets are required for prediction algorithms and for assessing needs
- Video and images – cameras are everywhere including CCTV, ANPR (automatic number plate recognition) cameras on main trunk roads, video doorbells that are connected to the Internet and smartphones. These could be used to augment GPS location data to help monitor activities or to analyse facial expressions and mood and social interactions.
- Speech – contextual information derived from how a person talks could be used to determine how much social interaction an individual has or potential mental health problems.
- Device use – the time spent on a smartphone and how it is used, including social media use, or watching TV could be used to monitor habits and changes in these.
While many smart technologies (like apps, websites, and smart TV’s) already monitor data such as which items someone is looking to buy or which TV programmes they like to watch, these types of intrusive monitoring techniques are controversial and generate serious privacy concerns, even when manufacturers claim that such data is anonymised. For this reason, their use within TEC applications is unlikely anytime soon.
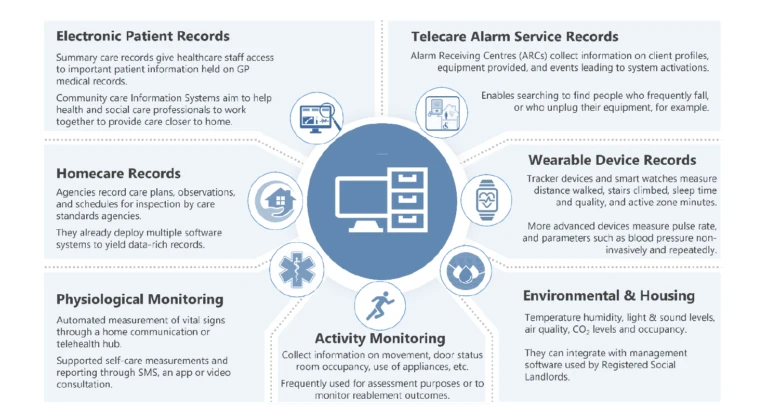
Figure 6: Example sources of electronic records.
As well as data generated by the person and their home, it is also desirable for other electronic records to be connected to a holistic care technology service data model, some examples of which are shown in Figure 6. However, one of the problems with such an approach is that there is not an agreed set of coding standards across all domains. In the health domain, there are standards in use that define how information is coded using a unified terminology (e.g. SNOMED CT) and shared across electronic health records and systems (HL-7 and FHIR, pronounced “fire” – a global industry standard framework describing data formats and elements together with an application programming interface for exchanging electronic health and care data between systems).
The increase in the availability of patient generated health data (PGHD) will have implications for both health informatics – so that it can be successfully integrated into electronic patient records – as well as security (how to link a disparate set of products and data to the system securely). With respect to activity monitoring applications, there are no agreed standards on how an individual’s activity data is recorded, although some technologies, such as Z-Wave, have standard profiles for individual sensors that allow for interoperability at the device level. The availability of an agreed coding standard for such data should be a priority for the sector.
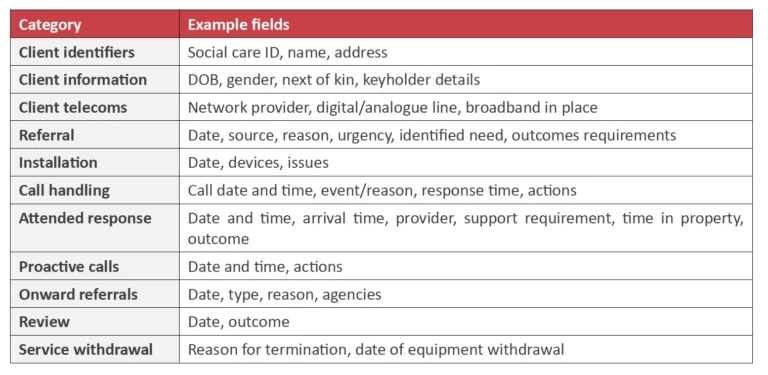
One area where work has begun in developing standards is with telecare service performance and outcome monitoring. Scotland has developed a telecare information framework that sets out to define a minimum data set for telecare services. Wales has also developed a minimum dataset and is involved in a collective procurement of alarm monitoring systems to support an improved interoperability agenda, though this is currently focussed on alarm-based telecare services.
Table 1: Data domains within the Scottish information framework for telecare services.
Conclusions
This article has discussed how technology-enabled care applications and services will increasingly rely on data rather than alarms. Data will be obtained from a wide range of sources:
- Sensors on the person (wearables) that monitor activity, health & wellbeing.
- Sensors in the home that monitor the person’s activities within the home including their interaction with furniture, fixtures, and individual appliances.
- Sensors in the home that monitor environmental conditions such as temperature, air quality and ‘global’ utility use (electricity, gas, and water).
- Data from apps and other connected devices that allow the user to provide answers in response to questions or if they have taken a health measurement (e.g., blood glucose level).
- Data from electronic records such as health and care records that can be used to help inform the service of important treatments, medications, interventions, issues and concerns, or changes in care or treatment plans.
- Unstructured sources including video, images, sounds, and responses to interactions with people, devices, and machines.
The service will also generate its own data, based on how it is used, performs and responds to need:
- A record of alerts and alarms generated by the system or raised manually by the person.
- A record of how the service or other people (e.g. family) or agencies (e.g. care services) have responded to requests for assistance.
- A record of outcomes based on interventions especially those instigated by the system. These data will be used to:
- Build a data model that provides a holistic overview of an individual’s health and wellbeing, allowing significant changes to be identified and future needs to be anticipated.
- Help assess the needs and capabilities of an individual and how these may be changing.
- Provide context-aware support to assist the individual with their day-to-day tasks.
- Monitor (and help control) their home environment to ensure that it is safe and comfortable.
- Generate alerts, alarms or perform automated actions if a serious problem is indicated.
- Monitor how the person uses technology and how often they are being helped by a monitoring/responder service (e.g. how their use of technology changes over time, the number of alerts/alarms generated, the number of times a response has been required and the nature of the response).
- How a technology-enabled care service is performing to ensure minimum standards are being met and to inform and monitor service changes for continuous improvement.
- Ensure that blended support services balance the use of technology with support delivered by people in the optimum way for the individual; and
- Build up evidence that shows what difference each specific intervention may have had to help establish their efficacy (or otherwise).
It is important to realise that the technology in the home required to support 3/4G+ applications is different from that currently being deployed to support 1/2G alarm-based services – this includes digital versions. Proactive and predictive services are built using consumer IoT sensors and platforms. These benefit from products that are pleasing to the eye, are low cost, and which use consumer smart home wireless technologies to link to a local hub or gateway/cell. It is likely therefore that sensors for use in care technology applications will become commodities. Any home hub may also become generic and interchangeable with value being provided higher up the stack from bespoke data analytics, machine learning algorithms, and simple-to-use data dashboards. Product differentiation within hubs could involve alternative user interfaces (UI) such as video and voice, with built-in intelligent voice assistants (such as the MiiCare MiiCube and their AI-powered voice assistant, Monica). Such capabilities may also be left to existing consumer technologies such as Amazon’s Alexa and Google’s Assistant. As discussed above, some sensors/devices may not need a local hub at all. What is certain, is that existing alarm-based telecare sensors are not, as currently configured, able to support 3G+ TEC applications. Service commissioners/providers should be mindful of this when developing their long-term strategies for using technology in care and support services.
Beyond the data obtained from sensors worn by an individual and installed in their home, 4G+ TEC platforms will make increasing use of data from other sources. Data models will increasingly incorporate additional qualitative and quantitative data from interactions with touchscreen applications, voice UI as well as external sources such as the wider Internet of Things and electronic health and care records. This is likely to also include health and fitness data from the growing consumer-based wearables and medical monitoring market.
Higher up the stack, the ability of the data analytics platform and associated algorithms to interpret data into meaningful information and useful alerts will be key to its success. Product suppliers are increasingly using machine learning to improve the automation of the data analysis process to generate higher-level information capable of instigating useful actionable insights for service providers. This will reduce the need for personnel to manually interpret disparate data streams to investigate issues. The simplicity of data dashboards and how well a platform can integrate data from external systems to provide a ‘single source of truth’ will be another key driver of success. The ‘linear’ responder model of 1/2G applications is giving way to a distributed model, where information is shared between various responders according to their need-to-know and ability to respond quickly.
These developments mean that the capabilities of the monitoring platform must adapt to be more open to accepting data from multiple sources and to be able to present that data in forms that are useful to the end-user. Discussions on these issues will be developed in a future article.
The next article will consider the changing landscape for the communication of data from devices to the cloud and to monitoring centres for analysis, coordination and response
Article written by T-Cubed
Sign up and keep up-to-date.
We'd love to keep you in the loop! Receive our latest news, events, insights, and blogs delivered straight to your inbox.

